Medical billing turns healthcare services into billable claims. It gets money back from insurance companies. This process is key to managing money in healthcare, linking patients, doctors, and insurance companies.
The medical billing process starts before coding and goes on until all money is paid back. Billers work with different groups, getting info, making claims, and handling payments. Making this work better is vital for healthcare to make more money, stay stable, and care for patients well.
Key Takeaways
- Medical billing is the linchpin of healthcare revenue cycle management, translating medical services into reimbursable claims.
- The billing cycle encompasses patient registration, insurance verification, claim submission, payment posting, and follow-up to ensure full reimbursement.
- Accurate medical coding and thorough documentation are essential for generating clean claims and minimizing denials.
- Leveraging technology solutions and adhering to compliance regulations are crucial for streamlining the medical billing process.
- Partnering with a trusted medical billing service provider can help healthcare organizations optimize revenue, improve efficiency, and enhance compliance.
Understanding Medical Billing and Healthcare Payment Systems
Medical billing is key in the healthcare world. It’s about sending claims to insurance companies for payment. It helps ensure healthcare providers get paid for their work. The main steps include registering patients, checking insurance, coding, sending claims, and processing payments.
Defining Medical Billing in Modern Healthcare
Medical billing handles the financial side of healthcare. It’s about sending claims to insurance companies for payment. This is crucial for healthcare organizations to stay financially healthy.
The Role of Medical Billing in Revenue Cycle Management
Medical billing is a big part of managing a healthcare organization’s finances. It covers everything from scheduling appointments to collecting payments. Good medical billing helps providers get the most money they deserve.
Key Components of Healthcare Payment Processing
The payment system in healthcare has several important parts:
- Insurance Eligibility Verification: Checking if a patient’s insurance covers the visit before it happens.
- Medical Coding: Turning services and diagnoses into codes for insurance companies.
- Claim Submission: Putting together all the needed info to send claims to insurance.
- Payment Posting and Reconciliation: Keeping track of payments from insurance and patients, and making sure everything adds up.
| Statistic | Value |
|---|---|
| Consumers Confused by Medical Bills | 72% |
| Consumers with Expensive Medical Bills | 94% |
| Claims Paid within 30-45 Days | Most States |
Managing these healthcare claims processing, insurance eligibility verification, medical coding, and revenue cycle management steps well is vital. It keeps healthcare organizations financially stable and patient satisfaction high.
Front-End Medical Billing Operations

The front-end of medical billing is all about patient-facing tasks. These tasks are key to accurate billing and managing revenue cycles. They include patient registration, insurance checks, and getting pre-authorization for services. Doing these tasks well helps avoid claim denials and boosts financial health.
Patient Registration and Data Collection
Getting patient information right is the first step in billing. Front-end staff need to collect patient details, insurance info, and medical history carefully. This info helps check if the patient is covered and who owes what, making claims more likely to pass.
Insurance Eligibility Verification
Before treatment, teams must check if insurance is valid, what’s covered, and what the patient owes. This step helps know what the patient can pay upfront, cutting down on denied claims and late payments.
Pre-Authorization Requirements
Many treatments need approval from insurance first. Front-end staff must know the rules for each insurance. Getting this approval before treatment ensures quick payment and less trouble with denied claims.
Improving front-end billing is key for a healthcare’s financial health. By making patient registration, insurance checks, and pre-approvals smoother, providers can make more money, reduce denials, and better the patient’s financial experience.
| Key Front-End Billing Activities | Importance |
|---|---|
| Patient Registration and Data Collection | Gathering accurate patient demographics, insurance coverage, and medical history is essential for verifying eligibility and generating clean claims. |
| Insurance Eligibility Verification | Confirming patient benefits, copays, and deductibles enables upfront point of service collections and reduces claim denials. |
| Pre-Authorization Requirements | Obtaining pre-approvals for services ensures timely reimbursement and minimizes administrative challenges associated with denied claims. |
“Automation of front-end revenue cycle processes can reduce errors and improve efficiency.”
Medical Coding and Documentation Requirements
In the complex world of healthcare, accurate medical coding is key. Medical coders turn diagnoses, procedures, and equipment into codes. These codes include ICD-10-CM for diagnoses, CPT for procedures, and HCPCS Level II for supplies and services.
Understanding medical terms, anatomy, and how the body works is crucial. Coders look through patient records to find the information needed for insurance claims. This step is vital for getting paid on time and correctly.
The quality of coding depends a lot on the documentation from healthcare providers. Poor or unclear documentation can cause coding mistakes. This can lead to claims being denied and lost revenue. Providers must make sure their records are detailed, clear, and show why services were needed.
Some common problems with documentation include:
- Insufficient progress notes or unauthenticated medical records
- Lack of documentation for the intent to order services
- Inadequate justification for the medical necessity of procedures, such as vertebral augmentation or physical therapy
- Incorrect coding of Evaluation & Management (E/M) services, including office visits, hospital visits, and insufficient documentation
- Incomplete documentation for Durable Medical Equipment (DME) orders, including missing standard written orders or face-to-face encounters
- Insufficient support for the medical necessity of Computed Tomography (CT) scans
To tackle these issues, healthcare providers should focus on detailed and accurate records. They should make sure all important information is included. Working well with coding and billing teams can help spot and fix any missing details. High-quality medical records help improve revenue cycle management and ensure timely payments.
The Medical Billing Process: Step-by-Step Workflow
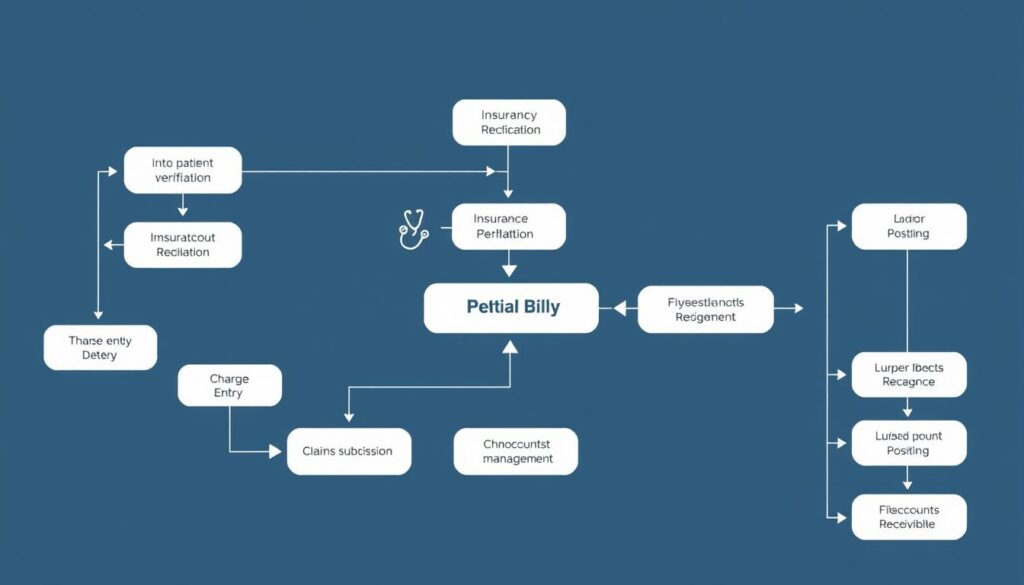
The medical billing process is key to the healthcare revenue cycle. It ensures payments are made on time and correctly. This process includes several steps, from capturing charges to posting payments.
Charge Entry and Claim Generation
The first step is charge entry, where providers document services given to patients. This info is then used to create a claim. The claim is a detailed request for payment sent to the patient’s insurance.
It’s important to code and document accurately at this stage. This helps avoid claim denials or delays in payment.
Claims Submission and Processing
After the claim is made, it’s sent to the payer or through a clearinghouse for processing. The adjudication process checks if the claim is covered and how much is owed. Claim scrubbing checks the claim’s accuracy to boost approval chances.
Payment Posting and Reconciliation
When a claim is approved, the provider gets paid. This payment is then recorded in the patient’s accounts receivable. This step is vital for keeping financial records accurate and collections on time.
If there are denials or underpayments, the billing team may appeal or bill the patient. Effective billing needs a deep understanding of the process and the use of technology. This helps streamline operations and improve charge capture and claim scrubbing.
By mastering this workflow, healthcare providers can manage their revenue better. This ensures the financial health of their practice.
| Key Steps in the Medical Billing Process | Description |
|---|---|
| Charge Entry | Healthcare providers document services rendered during patient encounters. |
| Claim Generation | Claims are created using coded information to request payment from insurance providers. |
| Claim Submission | Claims are submitted directly to payers or through a clearinghouse for processing. |
| Claim Adjudication | Payers review and determine coverage eligibility, payable amounts, and patient responsibilities. |
| Claim Scrubbing | Claims are verified for accuracy and completeness to minimize errors and increase approval rates. |
| Payment Posting | Reimbursements are recorded in the patient’s accounts receivable. |
| Reconciliation | Denials and underpayments are addressed through appeals or patient billing. |
By understanding the medical billing process, healthcare providers can make their revenue cycle more efficient. This improves their financial health and allows them to focus on patient care.
Insurance Claims Management and Reimbursement

Managing insurance claims well is key for healthcare providers. It ensures they get paid on time and correctly. This includes sending claims, checking their status, and dealing with denials or rejections.
Billers must follow up on claims that aren’t paid and handle appeals for denied ones. Once claims are approved, they work on getting paid back and keep track of money owed.
For patient bills, billers create statements and explain benefits. They tell patients about their financial duties. If patients don’t pay, billers might set up payment plans or use collection agencies.
Navigating Claim Denials and Appeals
Dealing with claim denials can slow down payments and add to workloads. Billers need to quickly find out why claims are denied and start the appeals process. This might mean getting more info, resubmitting claims, or talking to insurance companies.
Being proactive in managing claims helps healthcare providers keep more money and improve cash flow.
| Claim Denials | Appeals Process |
|---|---|
| – Incorrect coding or missing information – Non-covered services – Pre-authorization issues – Timely filing concerns |
– Gather supporting documentation – Resubmit the claim with additional details – Negotiate with the insurance provider – Follow up on the status of the appeal |
By getting good at managing insurance claims and getting paid, healthcare providers can do better financially. This way, patients can get the care they need without worrying about money.
“Effective claims management is essential for the financial health of any healthcare organization. It’s a critical component of the revenue cycle that requires specialized expertise and ongoing attention.”
Technology and Tools in Modern Medical Billing

Medical billing has changed a lot in the modern healthcare world. New technologies like electronic health records (EHRs) and practice management software have made it better. Now, billing is faster, more accurate, and safer.
Electronic Health Records Integration
EHRs have changed medical billing a lot. They mix patient data with billing info, making things smoother. This has cut down errors by 30% for some healthcare providers.
Practice Management Software Solutions
Practice management software is key in today’s medical billing. It handles things like scheduling and billing. It helps reduce claim denials by spotting problems early.
Claims Scrubbing and Verification Tools
Claims scrubbing tools check claims for mistakes before they’re sent. This makes sure they meet payer rules. It helps avoid denials and speeds up payments.
EDI systems are also changing medical billing. They make sending and getting claims fast and safe. This makes the whole payment process better.
Using new tech helps healthcare providers manage their money better. It cuts down mistakes and makes patients happier. As tech keeps getting better, it will be even more important for great healthcare.
| Technology | Benefits |
|---|---|
| Electronic Health Records (EHRs) |
|
| Practice Management Software |
|
| Claims Scrubbing and Verification Tools |
|
| Electronic Data Interchange (EDI) Systems |
|
“The integration of technology in medical billing has significantly boosted patient health outcomes and satisfaction levels.”
Compliance and Best Practices in Healthcare Billing

Keeping healthcare billing compliant is key for the medical system’s integrity and providers’ financial health. It means following rules like HIPAA for patient privacy and using best practices. These include accurate coding, proper documentation, and on-time claim submissions.
Staff training on coding and documentation is crucial. Regular audits to check billing practices are also important. Healthcare providers must keep up with policy and regulation changes to meet compliance.
Good documentation is essential for HIPAA compliance. It keeps patient info safe and shows services were needed. Following coding guidelines and documentation standards helps avoid fraud and abuse.
It’s vital to have ethical billing practices for the healthcare system’s financial health. Steps like a compliance hotline and thorough investigations of issues help. They prevent costly penalties and protect reputation.
By focusing on compliance and best practices, medical practices can offer quality care. They also keep their finances sound. This benefits both providers and patients.
| Compliance Requirement | Importance |
|---|---|
| HIPAA Compliance | Protects patient privacy and security |
| Coding Guidelines | Ensures accurate billing and prevents fraud |
| Documentation Standards | Demonstrates medical necessity and supports claims |
| Fraud Prevention | Maintains the integrity of the healthcare system |
“Compliance in health care billing helps prevent fraud, waste, and abuse in the system.”
Also Read : How Medical Technology Is Advancing Patient Care In Hospital Settings?
Conclusion
Effective medical billing is key for healthcare providers’ financial health. It covers everything from patient registration to final payment. Using efficient medical billing tech and following best practices are vital. This helps improve the revenue cycle and boosts patient satisfaction.
Keeping up with healthcare changes is crucial for success in healthcare financial management. By focusing on revenue optimization, providers can keep their operations running smoothly. This lets them focus on giving the best care to their patients.
In the end, good medical billing is essential for healthcare’s financial stability. It helps providers keep their finances strong, improve patient care, and help their communities thrive.
FAQs
Q: What is medical billing and coding?
A: Medical billing and coding is the process of translating healthcare services and procedures into standardized codes for billing purposes. This involves the use of coding systems, such as the Healthcare Common Procedure Coding System (HCPCS), to ensure accurate billing for services rendered to patients.
Q: What does a medical biller do?
A: A medical biller is responsible for preparing and submitting billing claims to insurance companies and ensuring that healthcare providers are compensated for their services. They also follow up on unpaid claims and manage patient billing inquiries.
Q: How can I become a medical biller?
A: To become a medical biller, you typically need to complete a medical billing and coding program, which may require an associate degree. Gaining experience in a medical office can also be beneficial. Obtaining certification, such as from the AAPC, can enhance your career prospects.
Q: What is a medical billing and coding program?
A: A medical billing and coding program is an educational course that trains individuals in the skills needed to work as medical billers and coders. This program covers medical terminology, coding systems, and billing procedures essential for success in the healthcare industry.
Q: What is the difference between a medical biller and a medical coder?
A: A medical biller focuses on the billing processes and payment collections, while a medical coder is responsible for translating healthcare services into standardized codes. Both roles are essential for the medical billing and coding process but focus on different aspects.
Q: Is there a certification for medical billing and coding professionals?
A: Yes, there are several certifications available for medical billing and coding professionals, including the Certified Professional Coder (CPC) and Certified Professional Biller (CPB) offered by the AAPC. These certifications validate the skills and knowledge required in the field.
Q: Can I take medical billing and coding courses online?
A: Yes, many institutions offer online medical billing and coding courses that provide flexibility for students. These online programs are designed to cover the same material as traditional in-person classes, allowing you to learn at your own pace.
Q: What is the job outlook for a career in medical billing?
A: The job outlook for a career in medical billing is positive, with the Bureau of Labor Statistics projecting growth in this field. As the healthcare industry expands, the demand for skilled medical billing and coding professionals is expected to increase.
Q: What skills are important for a medical billing and coding specialist?
A: Key skills for a medical billing and coding specialist include attention to detail, knowledge of medical terminology, proficiency with coding systems, and strong communication skills. These abilities are crucial for accurately processing billing claims and managing patient records.
Q: What is the role of health information in medical billing and coding?
A: Health information plays a critical role in medical billing and coding as it includes the patient’s medical records and details of the services provided. Accurate health information is essential for proper coding, billing, and ensuring compliance with healthcare regulations.
Source Links
- https://www.collaboratemd.com/blog/medical-billing-process/
- https://www.athenahealth.com/knowledge-hub/healthcare-technology/what-is-medical-billing
- https://www.drcatalyst.com/blog/the-medical-billing-process-101-everything-you-need-to-know/